Pulmonary imaging
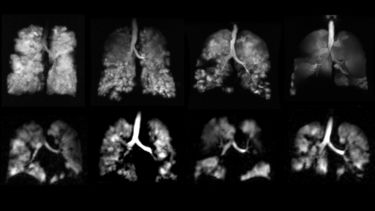
Our research focus is the application of magnetic resonance imaging (MRI) techniques to pulmonary diseases, with an overarching aim of developing novel imaging biomarkers that can be used to better understand the pathophysiology of lung disease.

Sheffield has pioneered the use of HP gas MRI over the last 20 years, and is a world leader in the field. In 2015 our centre was licensed for the manufacture of hyperpolarised 3He and 129Xe gas for clinical lung investigations, a world first for this technology.
This work has expanded significantly over recent years with the advent of a new imaging laboratory and now attracts clinical referrals from respiratory physicians across the UK.
Whilst inexpensive and simple to perform, spirometry is insufficiently sensitive to detect early functional changes associated with lung disease. More sensitive methods are needed to allow for early therapy and better patient management, and so we focus on applying hyperpolarised gas MRI to study lung microstructure, and ventilation and gas exchange function; high resolution structural MRI to visualise the lung macrostructure; and dynamic contrast enhanced MRI to assess lung perfusion. These methods can be applied to assess lung structure and function in a range of pulmonary disorders.
Research into these techniques is ongoing and areas of interest include:
- Chronic obstructive pulmonary disease (COPD)
- Asthma
- Interstitial lung disease (ILD), including Idiopathic Pulmonary Fibrosis (IPF)
- Cystic fibrosis (CF)
- Pulmonary vascular disease
- Pre-term birth-related lung disease and primary ciliary dyskinesia (PCD)
Overarching projects in clinical translation:
- Translating novel pulmonary MR imaging methods in to clinical practice. NIHR - Research Professorship. PI: Wild
- Expansion of state-of-the-art MR imaging infrastructure for pulmonary disease stratification: POLARIS. MRC - Resources and infrastructure Research Grant. PI: Wild
COPD and Asthma
Asthma and COPD are among the most common respiratory diseases, with COPD being the third leading cause of death worldwide. We use hyperpolarised gas MRI to visualise the distribution of ventilation in the lung and obtain imaging biomarkers of ventilation that show increased sensitivity over spirometry in COPD and asthma. Diffusion imaging can be used to measure enlarged alveolar airspaces in emphysema, and dynamic contrast enhanced perfusion imaging can visualise the distribution of blood perfusion in the lung microvasculature. In patients with severe COPD, time-resolved ventilation imaging can detect collateral ventilation, the key factor that determines the success or failure of lung volume reduction surgery (LVRS) using endobronchial valves.
Hyperpolarised gas MRI does not involve ionising radiation exposure and therefore can be performed repeatedly; e.g. multiple times in a single day to assess treatment response to bronchodilator therapy, or over longer time-periods to evaluate longer-term therapies. We have carried out studies to assess treatment response to novel drugs in patients suffering from these diseases. Furthermore, we have obtained Medicines and Healthcare products Regulatory Agency (MHRA) approval to perform these scans as part of routine clinical practice, to aid clinicians in managing those patients with challenging diagnoses. Our clinician collaborators report that visualising regional lung ventilation provides a greater clinical insight than spirometry alone.
Projects, Collaborators & Publications
- Current Projects / Grants
-
- ADPro NOVELTY study - Observational study of obstructive lung disease in patients with COPD and asthma (funded by AstraZeneca)
- Past Projects / Grants
-
- Study to assess the effect of Indacaterol/Glycopyrronium on ventilation and perfusion in COPD (funded by Novartis), EUDRACT # 2013-004461-13
- EU FP7 AirPROM - Airway Disease Predicting Outcomes through Patient Specific Computational Modelling
- Fevipripant asthma study with the University of Leicester (funded by EU FP7 Air PROM and Novartis)
- Investigation of the use of MRI to detect changes in ventilation-perfusion relationships in COPD (funded by GSK)
- Collaborators
-
- Rod Lawson (University of Sheffield)
- Ian Sabroe (Sheffield Teaching Hospitals)
- Chris Brightling and Salman Siddiqui (University of Leicester)
- Rod Hughes (AstraZeneca) Dave Singh and Rob Niven (University of Manchester)
- Key Publications
-
- Comparison of in vivo lung morphometry models from 3D multiple b-value 3 He and 129 Xe diffusion-weighted MRI. Chan HF, Collier GJ, Weatherley ND, Wild JM. Magn Reson Med. 2019 May;81(5):2959-2971. doi: 10.1002/mrm.27608.
- Comparison of 3 He and 129 Xe MRI for evaluation of lung microstructure and ventilation at 1.5T. Stewart NJ, Chan HF, Hughes PJC, Horn FC, Norquay G, Rao M, Yates DP, Ireland RH, Hatton MQ, Tahir BA, Ford P, Swift AJ, Lawson R, Marshall H, Collier GJ, Wild JM. J Magn Reson Imaging. 2018 Mar 5;48(3):632-42.
- Imaging Collateral Ventilation in Patients With Advanced Chronic Obstructive Pulmonary Disease: Relative Sensitivity of 3 He and 129 Xe MRI. Marshall H, Collier GJ, Johns CS, Chan HF, Norquay G, Lawson RA, Wild JM. J Magn Reson Imaging. 2019 Apr;49(4):1195-1197. doi: 10.1002/jmri.26273.
- Regional Ventilation Changes in the Lung: Treatment Response Mapping by Using Hyperpolarized Gas MR Imaging as a Quantitative Biomarker. Horn FC, Marshall H, Collier GJ, Kay R, Siddiqui S, Brightling CE, Parra-Robles J, Wild JM. Radiology. 2017 Sep;284(3):854-861. doi: 10.1148/radiol.2017160532.
- Direct visualisation of collateral ventilation in COPD with hyperpolarised gas MRI. Marshall H, Deppe MH, Parra-Robles J, Hillis S, Billings CG, Rajaram S, Swift A, Miller SR, Watson JH, Wolber J, Lipson DA, Lawson R, Wild JM. Thorax. 2012 Jul;67(7):613-7. doi: 10.1136/thoraxjnl-2011-200864.
Interstitial lung disease
Interstitial lung disease (ILD) covers a wide range of pulmonary disorders, including idiopathic pulmonary fibrosis (IPF) and hypersensitivity pneumonitis (HP), which can present as progressive fibrosis (scarring) of the lung tissue. ILD, whether fibrotic or not, is typically characterised by gas exchange functional impairment in the lung. The imaging methods that we use to help better assess the progression of disease in these patients include: diffusion-weighted MRI with hyperpolarised 3He or 129Xe, MR spectroscopy / spectroscopic imaging of 129Xe dissolved in the lung tissue and blood, and 1H dynamic contrast-enhanced (DCE) MRI. DW-MRI provides information on the microstructure of the alveoli, while 129Xe spectroscopy / spectroscopic imaging measures provide information on fibrosis and tissue thickening, and their influence on gas exchange. DCE MRI provides information on the passage of blood through the lung and its change over time in these patients. In addition, through recent collaborations with Wisconsin and the Mayo Clinic, we have implemented a high-resolution UTE MRI sequence for macrostructural assessment of the lung of comparable quality to CT, and have investigated quantitative CT biomarkers, in patients with ILD.
We are using high resolution UTE MR images to study patients with a number of subtypes of interstitial lung disease (ILD) as part of the TRISTAN study, and we are able to detect changes similar to those seen on CT.
Projects, Collaborators & Publications
- Current Projects / Grants
-
- Tristan: Using Imaging Biomarkers to Understand Potential Drug Side Effects in the Lung
- Investigation into prognostic indicators of Idiopathic Pulmonary Fibrosis using structural-functional pulmonary MRI assessment (funded by Boehringer Ingelheim)
- Assessment of lung function in patients with idiopathic pulmonary fibrosis using hyperpolarised xenon MRI, a sub-study of the ISABELA trial (funded by Galapagos)
- Collaborators
-
- Steve Bianchi (University of Sheffield)
- Steve Renshaw (University of Sheffield)
- Nazia Chaudhuri (University of Manchester NHS Foundation Trust)
- Paul Ford (Galapagos)
- Brian Bartholmai & Ronald Karwoski (Mayo Clinic; CALIPER Software)
- Kevin Johnson (University of Wisconsin)
- Joe Jacob (University College London, CALIPER analysis)
- Eric Hoffman (Iowa, AMFM quantitative ILD CT software)
- Key Publications
-
- Free breathing lung T1 mapping using image registration in patients with idiopathic pulmonary fibrosis. Saunders LC, Eaden JA, Bianchi SM, Swift AJ, Wild JM. Magn Reson Med. 2020 Dec;84(6):3088-3102.
- Hyperpolarised xenon magnetic resonance spectroscopy for the longitudinal assessment of changes in gas diffusion in IPF. Weatherley ND, Stewart NJ, Chan HF, Austin M, Smith LJ, Collier G, Rao M, Marshall H, Norquay G, Renshaw SA, Bianchi SM, Wild JM. Thorax. 2019 May;74(5):500-502.
- Airway Microstructure in Idiopathic Pulmonary Fibrosis: Assessment at Hyperpolarized 3He Diffusion-weighted MRI. Chan HF, Weatherley ND, Johns CS, Stewart NJ, Collier GJ, Bianchi SM, Wild JM. Radiology. 2019 Apr;291(1):223-229.
- Experimental validation of the hyperpolarized 129 Xe chemical shift saturation recovery technique in healthy volunteers and subjects with interstitial lung disease. Stewart NJ, Leung G, Norquay G, Marshall H, Parra-Robles J, Murphy PS, Schulte RF, Elliot C, Condliffe R, Griffiths PD, Kiely DG, Whyte MK, Wolber J, Wild JM. Magn Reson Med. 2015 Jul;74(1):196-207.
Cystic fibrosis
One key issue in monitoring patients with CF is the global information provided from lung function, rather than the locality and regional extent of lung disease, which can only be accessed with imaging. CT is often used clinically when managing patients with CF, however repeated exposure to ionising radiation, particularly in children, is a concern and has led our centre and others to pursue MRI for lung functional assessment of patients with CF.
We were the first centre to perform paediatric studies in CF, and have applied hyperpolarised gas and structural UTE MRI in CF in a number of studies, scanning patients as young as 6 years old. These imaging methods can detect subclinical changes in lung function and involve no ionising radiation, so are well-suited to longitudinal follow-up / monitoring of disease in these patients.
We are also involved in a number of collaborative studies investigating structure-function relationships in CF and evaluating novel proton MRI methods developed by our partners.
Projects, Collaborators & Publications
- Current Projects / Grants
-
- MMAVIC study - MRI & multiple breath washout to assess ventilation in cystic fibrosis
- VIPS study - Validation of bi- and three-dimensional Fourier Decomposition to assess lung ventilation and perfusion compared to CT, hyperpolarized gases and contrast-enhanced MRI
- Collaborators
-
- Chris Taylor (Sheffield Children’s Hospital)
- Noreen West (Sheffield Children’s Hospital)
- Alex Horsley (University of Manchester)
- Harm Tiddens (Erasmus MC, Rotterdam)
- Jens Vogel-Claussen (Hannover Medical School)
- Key Publications
-
- The effect of acute maximal exercise on the regional distribution of ventilation using ventilation MRI in CF. Smith LJ, Marshall H, Bray J, Wildman M, West N, Horsley A, Wild JM. J Cyst Fibros. 2021 Jul;20(4):625-631.
- The assessment of short and long term changes in lung function in CF using 129Xe MRI. Smith LJ, Horsley A, Bray J, Hughes PJC, Biancardi A, Norquay G, Wildman M, West N, Marshall H, Wild JM. Eur Respir J. 2020 Jul 6:2000441.
- Patterns of regional lung physiology in cystic fibrosis using ventilation magnetic resonance imaging and multiple-breath washout. Smith LJ, Collier GJ, Marshall H, Hughes PJC, Biancardi AM, Wildman M, Aldag I, West N, Horsley A, Wild JM. Eur Respir J. 2018 Nov 8;52(5):1800821.
- Longitudinal Assessment of Children with Mild Cystic Fibrosis Using Hyperpolarized Gas Lung Magnetic Resonance Imaging and Lung Clearance Index. Smith L, Marshall H, Aldag I, Horn F, Collier G, Hughes D, West N, Horsley A, Taylor CJ, Wild J. Am J Respir Crit Care Med. 2018 Feb 1;197(3):397-400.
- Detection of early subclinical lung disease in children with cystic fibrosis by lung ventilation imaging with hyperpolarised gas MRI. Marshall H, Horsley A, Taylor CJ, Smith L, Hughes D, Horn FC, Swift AJ, Parra-Robles J, Hughes PJ, Norquay G, Stewart NJ, Collier GJ, Teare D, Cunningham S, Aldag I, Wild JM. Thorax. 2017 Aug;72(8):760-762.
- Assessment of hyperpolarized 3He lung MRI for regional evaluation of interventional therapy: a pilot study in pediatric cystic fibrosis. Woodhouse N, Wild JM, van Beek EJ, Hoggard N, Barker N, Taylor CJ. J Magn Reson Imaging. 2009 Nov;30(5):981-8.
- Assessment of lung disease in children with cystic fibrosis using hyperpolarized 3-Helium MRI: comparison with Shwachman score, Chrispin-Norman score and spirometry. van Beek EJ, Hill C, Woodhouse N, Fichele S, Fleming S, Howe B, Bott S, Wild JM, Taylor CJ. Eur Radiol. 2007 Apr;17(4):1018-24.
- Hyperpolarized 3helium magnetic resonance ventilation imaging of the lung in cystic fibrosis: comparison with high resolution CT and spirometry. McMahon CJ, Dodd JD, Hill C, Woodhouse N, Wild JM, Fichele S, Gallagher CG, Skehan SJ, van Beek EJ, Masterson JB. Eur Radiol. 2006 Nov;16(11):2483-90.
- Quantitative analysis of regional airways obstruction using dynamic hyperpolarized 3He MRI-preliminary results in children with cystic fibrosis. Koumellis P, van Beek EJ, Woodhouse N, Fichele S, Swift AJ, Paley MN, Hill C, Taylor CJ, Wild JM. J Magn Reson Imaging. 2005 Sep;22(3):420-6.
Pulmonary vascular disease
Pulmonary vascular disease is diagnosed using invasive techniques such as right heart catheter or nuclear medicine imaging. Our research focus is the use of MRI for non-invasive diagnostic and prognostic markers in pulmonary vascular disease. We have developed image processing techniques and software to allow for analysis of quantitative metrics of cardiopulmonary function, such as pulmonary VQ matching and T1 relaxation time.
See also: Cardiovascular Imaging
Projects, Collaborators & Publications
- Current Projects / Grants
-
- CHANGE-MRI - CTEPH Diagnosis Europe
- Stratification and phenotyping of pulmonary vascular disease with imaging. Wellcome Trust Clinical Research Career Development Fellowship – PI: Swift
- Collaborators
-
- David Kiely (University of Sheffield)
- Roger Thompson (University of Sheffield)
- Charlie Elliot (University of Sheffield)
- Robin Condliffe (University of Sheffield)
- Allan Lawrie (University of Sheffield)
- Sheffield Pulmonary Vascular Disease Unit
- Jens Vogel-Claussen (Hannover Medical School)
- Key Publications
-
- Lung perfusion: MRI vs. SPECT for screening in suspected chronic thromboembolic pulmonary hypertension. Johns CS, Swift AJ, Rajaram S, Hughes PJC, Capener DJ, Kiely DG, Wild JM. J Magn Reson Imaging. 2017 Dec;46(6):1693-1697.
- Magnetic Resonance Imaging in the Prognostic Evaluation of Patients with Pulmonary Arterial Hypertension. Swift AJ, Capener D, Johns C, Hamilton N, Rothman A, Elliot C, Condliffe R, Charalampopoulos A, Rajaram S, Lawrie A, Campbell MJ, Wild JM, Kiely DG. Am J Respir Crit Care Med. 2017 Jul 15;196(2):228-239.
- Magnetic resonance imaging of ventilation and perfusion changes in response to pulmonary endarterectomy in chronic thromboembolic pulmonary hypertension. Marshall H, Kiely DG, Parra-Robles J, Capener D, Deppe MH, van Beek EJ, Swift AJ, Rajaram S, Hurdman J, Condliffe R, Elliot CA, Wild JM. Am J Respir Crit Care Med. 2014 Sep 1;190(5):e18-9.
- 3D contrast-enhanced lung perfusion MRI is an effective screening tool for chronic thromboembolic pulmonary hypertension: results from the ASPIRE Registry. Rajaram S, Swift AJ, Telfer A, Hurdman J, Marshall H, Lorenz E, Capener D, Davies C, Hill C, Elliot C, Condliffe R, Wild JM, Kiely DG. Thorax. 2013 Jul;68(7):677-8.
- Lung morphology assessment with balanced steady-state free precession MR imaging compared with CT. Rajaram S, Swift AJ, Capener D, Telfer A, Davies C, Hill C, Condliffe R, Elliot C, Hurdman J, Kiely DG, Wild JM. Radiology. 2012 May;263(2):569-77.
Pre-term Birth Related Lung Disease and PCD
In addition to our extensive research in to paediatric CF, we have utilised hyperpolarised gas MRI to study the lung ventilation and microstructural changes associated with pre-term birth related lung disease (Rhino study) and congenital diaphragmatic hernia (CDH).
In a study using ventilation MRI in children with primary ciliary dyskinesia (PCD), we found ventilation defects even in the presence of normal lung clearance index and FEV1, suggesting that ventilation MRI is a sensitive method for detecting lung disease in children with PCD.
Projects, Collaborators & Publications
- Current Projects / Grants
-
- RHiNO: Respiratory Health In Preterm Neonatal Outcomes
- ERS/EU Marie Curie Fellowship
- Thrasher Research Fund Early Career Award
- Collaborators
-
- Porus Bustani (Sheffield Teaching Hospitals)
- Sailesh Kotecha (Cardiff University)
- Jason Woods and Paul Kingma (Cincinnati Children’s Hospital Medical Center)
- Marjolein Spoel & Harm Tiddens (Erasmus MC, Rotterdam)
- Key Publications
-
- Imaging Lung Function Abnormalities in Primary Ciliary Dyskinesia Using Hyperpolarized Gas Ventilation MRI. Smith LJ, West N, Hughes D, Marshall H, Johns CS, Stewart NJ, Chan HF, Rao M, Capener DJ, Bray J, Collier GJ, Hughes PJC, Norquay G, Schofield L, Chetcuti P, Moya E, Wild JM. Ann Am Thorac Soc. 2018 Dec;15(12):1487-1490.
- Pulmonary ventilation and micro-structural findings in congenital diaphragmatic hernia. Spoel M, Marshall H, IJsselstijn H, Parra-Robles J, van der Wiel E, Swift AJ, Rajaram S, Tibboel D, Tiddens HA, Wild JM. Pediatr Pulmonol. 2016 May;51(5):517-24. doi: 10.1002/ppul.23325.
People
- Smitha Rajaram (Consultant Radiologist)