The FAIRSTEPS study
Framework to Address Inequities in pRimary care using STakEholder PerspectiveS
Background
Health inequities in UK primary care are the unfair and avoidable differences in access, experience and outcomes of healthcare services. These disparities are deeply rooted in wider social, economic and environmental factors. From language and cultural barriers to geographic disparities and digital exclusion; health inequities are widespread and fundamentally unfair.
By bringing together learning from patients with lived experience and frontline practitioners, the evidence-based University of Sheffield FAIRSTEPS framework is a tool to support the Primary Care sector to take action to increase equity.
The FAIRSTEPS study
The University of Sheffield-led Framework to Address Inequities in pRimary care using STakEholder PerspectiveS (FAIRSTEPS) produced a step-by-step framework and interactive toolkit to help primary care services reduce health inequities for their local populations. This was broken down into the local level - focusing on primary care practices and network - through to commissioners and primary care education.
The underpinning research involved reviewing existing studies, policies, and organisational websites. It also included gaining insights from healthcare professionals (such as frontline GPs and nurses) and developing a deep understanding of patient perspectives, working closely with the Deep End PPI group who represent communities from deprived areas in Sheffield.
Research outputs
- Step-by-step guide and prioritised actions for practices and networks, commissioners and educators
- An evidence-informed interactive toolkit for designing new local innovations
- An economic analysis demonstrating that most FAIRSTEPS prioritised interventions were both cost-effective and equity promoting
- Short report and user guidance
- Integrative evidence review and Delphi consensus - ScienceDirect
- Cost-effectiveness and equity impact of complex primary care interventions for disadvantaged populations
Our impact so far
The FAIRSTEPS framework has been endorsed by the popular primary care podcast eGPlearning, with a published research paper (insert link) being viewed thousands of times. The team has also presented at seven international conferences, presented to a national panel of senior healthcare managers for national dissemination and has run training courses with hundreds of trainee GPs.
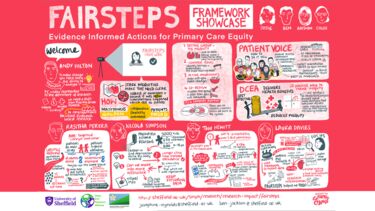
2025 FAIRSTEPS Masterclass
A FAIRSTEPS masterclass for primary care professionals in network leadership roles,, providing training and one-to-one support to empower the cohort to design bespoke localised interventions, is running throughout summer 2025.
You can view the short presentations from the Masterclass Showcase, click on the links below. These include presentations from one of our public participants on the importance of community engagement and our four participants on how useful they found FAIRSTEPS in developing health equity interventions for their own local populations.
MASTERCLASS Participants presentations
- Laura Davies: Equitable care in areas of high deprivation
- Rasitha Perera: Equitable preventative care interventions
- Tom Hewitt: Equitable care for people at high risk of hospital admission
- Nicola Simpson: Equitable asthma care for children
FAIRSTEPS team Masterclass presentations
- Ben Jackson: Introduction to the FAIRSTEPS method
- Josie Reynolds: Introduction to the FAIRSTEPS Masterclass
- Aaishah Aslam: Importance of meaningful public participation
- Chloe Thomas: Equity interventions and cost effectiveness
Building equitable primary care
In addition to the FAIRSTEPS framework as a stand alone tool, we collaborated with members of the EQUALISE study from Queen Mary's and Cambridge to produce a more in-depth PDF guide, which explores how to approach an intervention in more detail.
Building Equitable Primary Care
The FAIRSTEPS and EQUALISE studies were independent but had the same starting point - to reduce inequities we need to address the social determinants of health and interrogate power dynamics inside and outside primary care. Both studies combined expertise coming from social sciences, clinical healthcare and lived experience. They reviewed different, but complimentary literature, and came up with complementary findings, which were incorporated into the Building Equitable Primary Care toolkit.
It provides further information about how the two studies aligned and presents their findings in the context of real-life examples of effective models and interventions from the UK and beyond.
Testimonials
Patients and collaborators from primary care share how they have helped to shape the FAIRSTEPS framework:
The opportunity to be involved in the FAIRSTEPS work was a huge privilege but seeing the quality of the output is what made this collaborative endeavour so rewarding. The FAIRSTEPS framework is a game-changer and an enabler for all those wishing to meaningfully address inequities in primary care.
Dr Nigel Hart
GP in Northern Ireland and Professor of General Practice
I enjoyed working on the FAIRSTEPS study because I liked hearing the views of others and working with the information to develop the framework together. I learnt that we all have something to give and even if we have differing views, it's all useful.
Carole Hobson
Deep End Patient Public Involvement (PPI) contributor
As a PPIE member for the FAIRSTEPS study – my most meaningful and favourite part was when we helped shape priority interventions for networks and practices; primary care commissioners; and education and training providers. This was done through several meetings discussing vignettes where we openly and vigorously shared our views and lived experiences and community perspectives discussing services and interventions that would realistically benefit patients and be culturally appropriate with local communities, often underrepresented and commonly unable to access health and care services. All the researchers, especially Ben, were extremely welcoming, polite and non-judgemental, and this was a key factor in wanting to get more involved in the study.
Aaishah J-Aslam
Deep End Patient Public Involvement (PPI) contributor
Resources
Practical steps to reduce inequalities in primary care - Health Equity Evidence Centre
Contact
To find out more or get in touch about FAIRSTEPS, or if you want to enquire about support for a FAIRSTEPS workshop in your area or within your organisation, please contact Dr Josephine Reynolds or Professor Ben Jackson.