Bridging cultures in mental health
1 in 4 people will experience struggles with their mental health in the course of a year. But cultural sensitivities and language differences put up barriers for many patients. Sheffield researchers have developed a training course to deepen the cultural understanding of healthcare professionals.

1 in 4 people will experience struggles with their mental health in the course of a year. There are a number of ways to seek support (see end of the article) and it is recommended that if you notice changes in the way you are thinking or feeling over a period of weeks or months that concern you, you should consider going to see your GP.
Talking about mental health is already a difficult and sensitive topic for many, particularly as we often find ourselves needing to talk about it when we are not feeling so good. But cultural and linguistic differences can create a bigger distance between service users and health care professionals which means it isn’t as straightforward for everyone to receive the support and care they need.
Census data published in 2021 shows that England and Wales are more ethnically diverse, and less segregated than ever before. Sheffield is a multicultural city and areas such as Netherthorpe, Upperthorpe and Neepsend are some of the most diverse neighbourhoods with a Black, Asian and minority ethnic population of 31.9 per cent.
According to the Royal College of GPs, an average patient will see a GP around seven times a year. However, a report led by The Healthcare Safety Investigation Branch (HSIB) found that patients whose first language is not English have a heightened risk of not attending the appointment at all. With GPs encountering patients from different cultural and religious backgrounds, language barriers and social problems, such as racism, often lead to reduced patient engagement with mental health services.
Language carries different cultural meanings. In Sheffield alone, over 120 languages are spoken but people from different cultural backgrounds who are experiencing distress can be at a disadvantage. While it is not possible to learn about all cultural backgrounds, researchers at Sheffield are taking a collaborative approach to provide health and social care practitioners with the tools to improve intercultural communication and understanding in healthcare.
Dr Jane Woodin is the Programme Leader for MA in Intercultural Communication and Senior University Teacher in the School of Languages and Cultures at the University of Sheffield. She first met Dr Nahed Arafat while supervising her Masters dissertation and later her thesis in Intercultural Communication. Nahed is a Mental Health Practitioner and Research Assistant at the University of Sheffield. Combining Jane’s expertise in intercultural linguistics and Nahed’s lived experience as Mental Health Professional and interpreter in Sheffield, the pair have developed and led a Continuing Professional Development (CPD) course to enhance the cultural competence of health and social professionals in Sheffield.
“Your lived experience such as the languages you speak, your educational and religious upbringing together with political realities such as conflicts in your country of origin will have affected the way that you see the world in some way. Our training helps professionals to relativise their views and be able to easier adopt the perspectives of others to help provide an improved service to patients” explains Jane.
Providing training
Continuing Professional Development (CPD) is the process of developing and updating knowledge, expertise and competence to increase your knowledge of a subject area or role. In healthcare, this leads to providing the best possible service for patients.
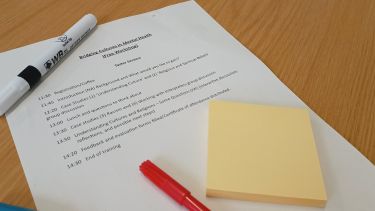
Following Jane and Nahed’s highly successful taster session offered to Health and Social care professionals on the Arts and Humanities Knowledge Exchange project ’Bridging Cultures in Mental Health’ (2021-2022), Nahed was commissioned by the Health and Social Care Trust to offer 12 cultural awareness training workshops for professionals in Sheffield. The workshops are tailored to encourage professionals to engage in the discovery, analysis and reflection of their work with patients from diverse backgrounds.
Based on Nahed's own experience and PhD research own experience and research into intercultural issues in the healthcare sector, the training content was designed to help professionals deepen their sensitivity towards patients. This included developing an understanding of the unique mental health needs of immigrants, raising awareness of institutional racism and its impact on patients from minority groups and creating a safe space for sharing and reflecting on their work experiences with colleagues.
The training started with a sharing session where participants were divided into groups to discuss the main challenges they encounter when working with patients from diverse backgrounds, and how those challenges affect their relationships with patients.
This was followed by a guided imagery exercise, where participants heard first-hand experiences of patients’ experiences and the reasons why they felt unable to engage with mental health services.
The exact content of the workshops can vary, but a typical 3-hour workshop would cover four case studies about culture, religion, working with interpreters and racism. These topics would vary depending on the roles of the participants, and end with a discussion about white supremacy.
The training was delivered in face-to-face sessions to encourage participants to discuss their experiences openly. All training activities used case studies adapted from real-life case studies to encourage members to challenge their beliefs, prejudices and stereotypes. In addition to the Training workshop, participants are invited to take part in a follow-on hour to reflect on the information received and share views on how this will impact their practice.
“We added a reflective session to receive feedback from the participants to learn how the training related to participants' everyday work as well as to learn more about possible future developments. Our Research Assistant, Amanda Tavares, who led these sessions, was incredibly engaging and helped to shed light on the training from an external perspective. We received positive feedback about the reflective sessions as it allowed participants to think about what they took away from the training and some suggested making it part of the CPD training” explains Nahed.
“One of the best outcomes to come from the training was that participants felt more confident in asking personal questions without feeling like they were offending or being ignorant. This is precisely what we wanted as it reduced the risk of creating assumptions about a patient” she adds.
In total, 77 participants from Sheffield Health and Social Care Trust, including managers and practitioners of all roles, such as admins, nurses, social workers and therapists engaged to date in the training.
Growing confidence in dealing with intercultural issues
Overall, participants expressed becoming more knowledgeable and aware of the complex issues of refugees and asylum seekers and how cultural backgrounds, and religious and spiritual beliefs can impact a patient’s engagement with healthcare.
76 per cent of participants found the materials and training thought-provoking, engaging and helpful and reported motivation to continue having open discussions into work-related practices in other areas of mental health.
Participants said they felt more confident asking questions about cultural and religious beliefs they were unaware of, as well as feeling better equipped to meet patients’ needs and encourage them to talk about their trauma and share their experiences. Some expressed their intention to reserve more time when meeting patients with interpreters, as well as discussing the contents of the training with their colleagues, to further develop cultural awareness in their roles and reinforce good practices.
The majority of participants reported a growth in confidence in dealing with intercultural issues, asking questions and being inquisitive about topics they do not understand. Many participants praised the safe space created and sustained during the training, which helped them share experiences and feel comfortable to ask questions. A small number of healthcare professionals were able to cite specific instances where the training had connected to a real-life experience between the training and the reflection session.
It’s made me more conscious of people’s backgrounds, of where people have come from and the difficulties that they’ve had in terms of having to come to this country, and having to deal with difficult situations and not knowing where to go
Training participant
Many participants voiced the need for this training to be mandatory for the entire Trust and stated that this training was very different from others they had previously attended.
Looking ahead
Participants asked for further training sessions on the perceptions and explanations of mental health in different cultures, how to introduce new policies to respond to patients’ needs more effectively, and best practices when working with interpreters.
Jane and Nahed are now evaluating ways to reach more healthcare professionals with this training with a focus on delivering in-person sessions.
“The face to face element is a core element of this training. After a guided imagery session, one woman said it gave her goosebumps as she felt like she was in the patient’s shoes. It’s difficult to replicate this powerful feeling through digital training” explains Nahed.
“Most people find training a boring admin task. As opposed to mandatory training, our interactive sessions are designed for professionals to attend as and when necessary. This helps participants to engage with the information and discussion when needed and develop cultural and interpersonal skills, rather than sitting through a lecture” Nahed adds.
Based on the feedback from these sessions, the team are in the process of developing further Cultural Awareness training to reach more members of the Sheffield Health and Social Care Trust and beyond. There are also discussions about how to disseminate the learnings from this project, such as publishing materials to become more widely available and offering further CPD courses in the future.
Written by Alina Moore, Research Communications Coordinator
Support information
If you’ve been affected by any of the issues in this article, please contact your GP or the following organisations:
Samaritans
To talk about anything that is upsetting you, you can contact Samaritans 24 hours a day, 365 days a year.
Call: 116 123
SANEline
If you're experiencing a mental health problem or supporting someone else, you can call SANEline on 0300 304 7000 (4.30pm–10.30pm every day).
Call: 0800 689 5652 (6pm to midnight every day).
Campaign Against Living Miserably (CALM).
You can call the CALM if you are struggling and need to talk. Or if you prefer not to speak on the phone, you could try the CALM webchat service.
Call: 0800 58 58 58 (5pm–midnight every day)
Shout
If you would prefer not to talk but want some mental health support, you could text SHOUT to 85258. Shout offers a confidential 24/7 text service providing support if you are in crisis and need immediate help.
For further information contact:
mediateam@sheffield.ac.uk