- Macrophages are key immune cells to clear pathogens at early stages of infection and also repair damaged tissues
- The study finds a significant decline in the ability of macrophages to engulf foreign particles, mimicking bacteria and viruses and migrate towards sites of infection to fight the invading pathogen in older adults compared to younger individuals
- The authors identify two master-regulator genes, MYC and USF1 that decline with age and may be responsible for the weakened macrophage function in older adults
- These findings present an opportunity to develop targeted treatments for enhanced macrophage function and potentially lead to an improved immune response in old age
Research from the Healthy Lifespan Institute offers a significant breakthrough in understanding age-related immune decline.
A fully functioning immune system is essential to help the body maintain good health, and macrophages play a critical role in maintaining robust immune responses against infections.
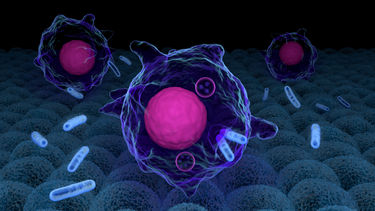
A macrophage is a type of white blood cell that kills microorganisms, removes dead cells, and stimulates the action of other immune cells. These cells play a critical role in the initiation, maintenance, and resolution of inflammation but undergo functional decline and deteriorate the immune system with age. This leads to increased susceptibility to infection and autoimmunity in the older population.
A new study, funded by the Healthy Lifespan Institute and the Faculty of Health at the University of Sheffield, published in Cell Reports, for the first time, identified that defects in macrophage function are driven by MYC and USF1 transcriptional programmes.
The research, led by Charlotte Moss, Dr Heather Wilson and Professor Endre Kiss-Toth has identified a potential culprit for this decline: two critical molecules within macrophages, MYC and USF1, which appear to act as malfunctioning "dimmers" with age.
Macrophages, often referred to as the body's garbage trucks, are responsible for engulfing and eliminating foreign particles, including debris and pathogens. The study demonstrates a significant reduction in the effectiveness of macrophages isolated from older adults compared to those from younger individuals. These aged macrophages exhibited diminished phagocytosis, the process of engulfing foreign particles, and impaired chemotaxis, their ability to migrate towards threats.
Strengthening this connection, the researchers artificially reduced MYC and USF1 activity in young macrophages. This manipulation resulted in a functional decline that mirrored the characteristics observed in macrophages from older adults. This finding strongly suggests that MYC and USF1 play a crucial role in maintaining optimal macrophage function.
The study ventures beyond simply identifying the culprits. It explores how the decline in MYC and USF1 activity might be impacting macrophages. The researchers posit that these changes may disrupt genes responsible for the cell's internal cytoskeleton, a network of filaments that provides structure and facilitates movement. This disruption could hinder the macrophage's ability to move and engulf foreign particles. Additionally, altered MYC and USF1 activity might affect how macrophages interact with their surrounding environment, further compromising their ability to combat infection.
This research offers a significant breakthrough in understanding the mechanisms of age-related immune decline.
By identifying MYC and USF1 as potential culprits, the study paves the way for the development of novel therapeutic strategies. By targeting these molecules or their downstream gene products, researchers might be able to enhance macrophage function in older adults, potentially leading to a more robust immune response and improved resistance to infection.
It is important to acknowledge that the study involved healthy volunteers and did not encompass individuals with pre-existing age-related illnesses. Additionally, the research was conducted in a controlled laboratory setting. Further studies are necessary to validate these findings in a broader population and explore the feasibility of translating these discoveries into effective therapies.
The identification of MYC and USF1 as potential targets for intervention represents a significant step forward. This research holds promise for the development of future strategies to bolster the immune system in older adults, ultimately contributing to healthier ageing.
“Understanding why the immune system is no longer effective in fighting off infections in old age is key to be able to develop treatments that may be able to reverse this decline. Our work is the first to uncover the molecular details of ageing in human phagocytes and we believe that this new understanding now gives us ways to test the effectiveness of various interventions, including diet, lifestyle and even potential drugs that aim to reverse age-related immune decline ” says Endre Kiss-Toth.
For media enquiries please contact mediateam@sheffield.ac.uk