Pre-clinical research
Our pre-clinical research is working to understand the underlying mechanisms of dementia so that we can identify new targets for therapies.
Our pre-clinical research is investigating the underlying biological mechanisms of dementia. By gaining a better understanding of the disease we are identifying new therapeutic targets.
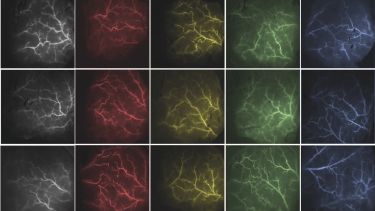
Researchers specialise in in vitro and in vivo modelling as well as sophisticated multi-modal imaging and neural recording techniques.
Our facilities can measure brain function from single cell (2-photon microscopy) up to whole brain (Magnetic resonance imaging) to provide accurate readouts of disease progression and test the effect of new therapies.
Our research
Using models of Drosophila melanogaster (fruit flies) in the mechanisms of frontotemporal dementia
Frontotemporal Dementia (FTD) is the second most common cause of early-onset dementia - affecting people under 65 years of age. Our research uses the unrivalled genetic tractability of Drosophila as a model organism to unravel the molecular mechanisms underpinning neurodegeneration in FTD.
We have developed the first in vivo models expressing pathological dipeptide-repeats (DPR) associated with C9orf72 related FTD of a length comparable to those observed in patients. Our current work looks to determine how each DPR contributes towards neurodegeneration, individually and in combination. Utilising the rapid generation time and short lifespan of Drosophila we have established a number of drug screening assays that allow us to monitor the effect of drugs from cell to behaviour in an ageing in vivo system.
Contact: Dr Ryan West
Investigating how changes in blood flow in the brain can be a factor in early models of dementia
A drop in blood flow to the brain is thought to be one of the causes of dementia so we are developing new strategies to enhance the blood supply. We have recently shown that we can dramatically increase blood flow across the brain by giving pure oxygen in a young pre-clinical Alzheimer’s model.
We have found that stimulation of a small group of interneurons in the brain dramatically increases brain blood flow without increasing metabolic demand. We plan to use this method to regularly enhance blood flow in our pre-clinical models to reduce disease burden.
As one of the highest risk factors for dementia is heart disease, we have developed preclinical models that have both conditions and have shown that these models have increased neuroinflammation in the brain. Future research will test whether a reduction in neuroinflammation can slow the progression of these diseases.
Contact: Dr Jason Berwick
The Sheffield Neurovascular Lab
Transcriptomic profiling as a method to identify relevant gene expression changes associated with ageing and dementia
In addition to performing detailed histological characterisation of post-mortem tissue, the neuropathology group uses transcriptomic profiling techniques, including microarray analysis and RNAseq, to identify specific gene expression changes and biological processes associated with ageing and dementia.
Age-associated periventricular white matter lesions are significantly associated with cognitive decline in the ageing population. Our recent study characterising their gene expression profile suggests that increased glutamate and calcium signalling may be a neuroprotective mechanism to prevent the formation of these lesions.
Neutrophils are key players of the immune response and, when activated, produce neutrophil-derived microvesicles. We have recently shown that internalisation of these microvesicles by brain endothelial cells in vitro decreases the expression of genes which regulate vascular integrity. These findings suggest that neutrophil-derived microvesicles may play an important role in modulating the permeability of blood-brain barrier during an infection.
Contact: Dr Julie Simpson
Investigating how metabolism in different types of brain cells and peripheral patients’ cells may be targeted to develop new therapeutics and biomarkers for dementia
Changes in cellular metabolism are seen early in Alzheimer’s disease and other dementias. These changes are likely to be caused by a combination of factors which benefit from being studied in cellular models derived from patients with dementia. Understanding the changes to metabolism in more detail in dementia has the potential to allow the development of both new biomarkers of dementia and treatments.
Our research uses different cell models to study the metabolism in both peripheral and nervous system cells in Alzheimer’s disease and other dementias. We use our understanding of metabolic abnormalities in dementia patient cells to test potential drugs in these cell models. In addition we investigate the metabolic relationship between different types of brain cells. We use a technology that reprograms fibroblast cells taken from patients with dementia into both neurons and astrocytes and then investigate the changes to glycolysis, mitochondrial function and lipid metabolism in these cells.
The cell models we use benefit from maintaining both an age phenotype, and having a great wealth of clinic data to accompany the research samples.
Contact: Dr Simon Bell and Dr Heather Mortiboys
Key academic staff
Partner with us
We are proud to work in collaboration with other organisations to seek new and exciting opportunities to further enhance our research.
- Well characterised pre-clinical models of dementia can produce stable and reproducible results and offer an opportunity to develop drug discovery and industrial collaborations.
- Unique, Drosophila models of dementia provide a fast and robust model for in vivo drug screens.
- We have established collaborations in this area and welcome contacts to initiate new collaborations.
To find out more contact Dr Jason Berwick.
-
Key publications
-
Ajikumar A, Long MB, Heath PR, Wharton SB, Ince PG, Ridger VC, Simpson JE (2019) Neutrophil-derived microvesicle induced dysfunction of brain microvascular endothelial cells in vitro. International Journal of Molecular Sciences 20(20) pii: E5227.
Allen S, Singh Seehra R, Hall BPC, Heath PR, Bates J, Garwood C, Matuszyk M, Wharton SB, Simpson JE (2020) Transcriptomic analysis of human astrocytes in vitro reveals hypoxia-induced mitochondrial dysfunction, modulation of metabolism and dysregulation of the immune response. Int J Mol Sci. 21(21):E8028.
Ameen-Ali K, Simpson JE, Wharton SB, Heath PR, Sharp P, Brezzo G, Berwick J (2019) The time course of recognition memory impairment and glial pathology in the hAPP-J20 mouse model of Alzheimer's disease. Journal of Alzheimer’s Disease 68(2):609-624.
Ameen-Ali K, Simpson JE, Wharton SB, Heath PR, Sharp PS, Brezzo G & J Berwick (2019). The Time Course of Recognition Memory Impairment and Glial Pathology in the hAPP-J20 Mouse Model of Alzheimer's Disease. J Alzheimers Dis. 2019;68(2):609-624.
Ameen-Ali K, Wharton SB, Simpson JE, Heath PR, Sharp P & Berwick J (2017). Review: Neuropathology and behavioural features of transgenic murine models of Alzheimer's disease. Neuropathol Appl Neurobiol. 2017 Dec;43(7):553-570.
Bell, M. S., De Marco, M., Barnes, K., Shaw, J. P., Ferraiuolo, L., Blackburn, J. D., Mortiboys, H.*, and Venneri, A*. (2020). Deficits in Mitochondrial Spare Respiratory Capacity Contribute to the Neuropsychological Changes of Alzheimer’s Disease. Journal of Personalized Medicine 10. * joint senior authors
Bell, S. M., Barnes, K., Clemmens, H., Al-Rafiah, A. R., Al-Ofi, E. A., Leech, V., Bandmann, O., Shaw, P. J., Blackburn, D. J., Ferraiuolo, L., and Mortiboys, H. (2018). Ursodeoxycholic Acid Improves Mitochondrial Function and Redistributes Drp1 in Fibroblasts from Patients with Either Sporadic or Familial Alzheimer's Disease. Journal of molecular biology 430, 3942-3953.
Fadul MM, Heath PR, Cooper-Knock J, Kurtz J, Al-Azzawi H, Ali Z, Smith T, Matthews FE, Brayne C, Wharton SB, Simpson JE (2020) Transcriptomic analysis of age-associated periventricular lesions reveals dysregulation of the immune response. Int J Mol Sci. 21(21):E7924.
Goodall EF, Leach V, Wang C, Cooper-Knock J, Heath PR, Baker D, Drew DR, Saffrey MJ, Simpson JE, Romero IA, Wharton SB (2019) mRNA and miRNA expression changes at the neurovascular unit reveal a role for autophagy and DNA binding in the cerebral microvasculature of the ageing brain. International Journal of Molecular Sciences 20(12) pii: E3097.Lee L, Boorman L, Glendenning E, Christmas C, Sharp P, Redgrave P, Shabir O, Bracci E, Berwick J & Howarth C (2020). Key Aspects of Neurovascular Control Mediated by Specific Populations of Inhibitory Cortical Interneurons. Cereb Cortex. 14;30(4):2452-2464
Lu Y, West RJH, Pons M, Sweeney ST, Gao FB. Ik2/TBK1 and Hook/Dynein, an adaptor complex for early endosome transport, are genetic modifiers of FTD-associated mutant CHMP2B toxicity in Drosophila. Sci Rep. 2020
Shabir O, Berwick J, Francis SE. (2018) Neurovascular dysfunction in vascular dementia, Alzheimer’s and atherosclerosis. BMC Neuroscience 19:62.
Shabir O, Moll TA, Matuszyk MM, Eyre B, Dake MD, Berwick J, Francis SE (2020). Preclinical models of disease and multimorbidity with focus upon cardiovascular disease and dementia. Mechanisms of Ageing and Development,192,111361
Shabir O, Sharp P, Rebollar MA, Boorman L, Howarth C, Wharton S, Francis SE, Berwick J (2020). Enhanced Cerebral Blood Volume under Normobaric Hyperoxia in the J20-hAPP Mouse Model of Alzheimer’s Disease. Scientific Reports, 10, 7518.
Sharp PS, Ameen-ALi KE, Boorman L, Harris S, Wharton S, Howarth C, Shabir O, Redgrave P, Berwick J. (2019). Neurovascular coupling is preserved in a chronic mode of Alzheimer's Disease: Methodology is critical. Journal of Cerebral Blood Flow and Metabolism, 271678X19890830.
Sharp PS , Shaw K, Boorman L, Harris S, Kennerley AJ, Azzouz M & Berwick J (2015). Comparison of stimulus-evoked cerebral hemodynamics in the awake mouse and under a novel anesthetic regime. Sci Rep. 2015 Jul 28;5:12621.
West RJH*, Sharpe JL, Voelzmann A, Munro AL, Hahn I, Baines RA, Pickering-Brown S. Co-expression of C9orf72 related dipeptide-repeats over 1000 repeat units reveals age- and combination-specific phenotypic profiles in Drosophila. Acta Neuropathol Commun. 2020 Sep 7;8(1):158.
*corresponding author
West RJH, Ugbode C, Fort-Aznar L, Sweeney ST. Neuroprotective activity of ursodeoxycholic acid in CHMP2BIntron5 models of frontotemporal dementia. Neurobiol Dis. 2020 Oct;144:105047.
West RJH, Ugbode C, Gao FB, Sweeney ST. The pro-apoptotic JNK scaffold POSH/SH3RF1 mediates CHMP2BIntron5-associated toxicity in animal models of frontotemporal dementia. Hum Mol Genet. 2018 Apr 15;27(8):1382-1395.
West RJH, Lu Y, Marie B, Gao FB, Sweeney ST. Rab8, POSH, and TAK1 regulate synaptic growth in a Drosophila model of frontotemporal dementia. J Cell Biol. 2015 Mar 30;208(7):931-47.
